New targets for brain cancer
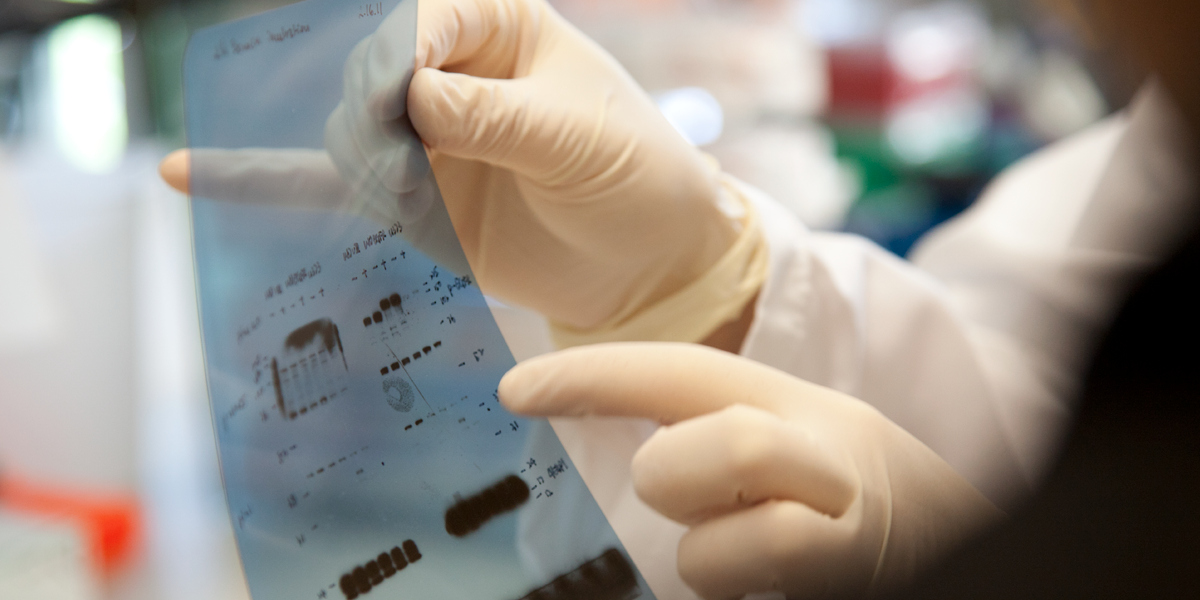
Researchers are exploring ways that combination therapies can treat glioblastoma.
If any tumor type is a candidate for combination therapy, it is glioblastoma multiforme. This aggressive brain cancer defies most treatment strategies. Chemotherapy barely touches it, and drugs that target cancer-causing cellular molecules are also remarkably ineffective in treating it. Median survival is 15 months after diagnosis.
Ludwig has long supported research programs to tackle this disease. Recently, physician-scientist Paul Mischel, a former faculty member at the University of California, Los Angeles, was recruited to the Ludwig San Diego team. He has helped design and lead molecular analysis in five clinical trials of therapies targeting cancer-related cellular molecules. Mischel’s expertise complements a team with strengths in basic research. It includes geneticist Frank Furnari and Ludwig San Diego director Web Cavenee, who study the diverse cellular mechanisms that drive cancer.
Mischel’s move to Ludwig last fall was a natural evolution of an ongoing longdistance interaction with Furnari and Cavenee. “We have shared interests and complementary approaches,” says Mischel. “The synergies among us were so great that it made sense to work closer together.”
One of the trio’s most recent projects delved into why two drugs designed to inhibit a cellular molecule called epidermal growth factor receptor (EGFR) work poorly in patients with glioblastoma. EGFR inhibitors such as these two, erlotinib and gefitinib, are effective in many patients with breast and other cancers. But less than 10 percent of glioblastoma patients respond to the drugs, and when they do, the response is usually short-lived. In figuring out why this happens, the researchers hope to find new ways to combine EGFR inhibitors with other agents to treat glioblastoma and other cancers.
The new study built on previous research pioneered by Mischel in partnership with Cavenee and Furnari. The three have shown that many people with the tumor have defects in a molecule called PTEN, enabling tumor cells to circumvent the drugs. In some unresponsive patients the gene encoding PTEN is mutated. But other unresponsive patients have normal PTEN, suggesting that the molecule can be deactivated in another way.
Last year, the team discovered a new mechanism of PTEN deactivation. They found that the molecule can be inactivated by a molecular modification — the addition of a phosphate molecule. Testing clinical samples obtained by Mischel and Ludwig collaborators in São Paolo, Brazil, the researchers found that PTEN phosphorylation is associated with resistance to EGFR inhibitors and shortens overall patient survival. Experiments on cancer cells in a test tube similarly showed that PTEN phosphorylation leads to resistance to EGFR inhibitors.
The team also identified some of the cellular regulators that add a phosphate group to PTEN. They are now identifying regulators that remove the phosphate group. The researchers ultimately aim to test whether interfering with one of these regulators, for instance targeting them with a small druglike agent, could reactivate PTEN in tumors. Such an agent could form the basis of a drug to be used in combination with an EGFR inhibitor. The findings were published in Proceedings of the National Academy of Sciences.
“We need to fully understand how this mechanism works, and we’re hoping these new findings will move us into clinical trials,” says Cavenee. This is something Mischel, with his extensive experience in the clinic, is well prepared to do in collaboration with his new San Diego colleagues. Says Cavenee, “We are constantly walking into each other’s off ices and bouncing ideas off of one another. I should have hired Paul years ago—but better late than never!”