
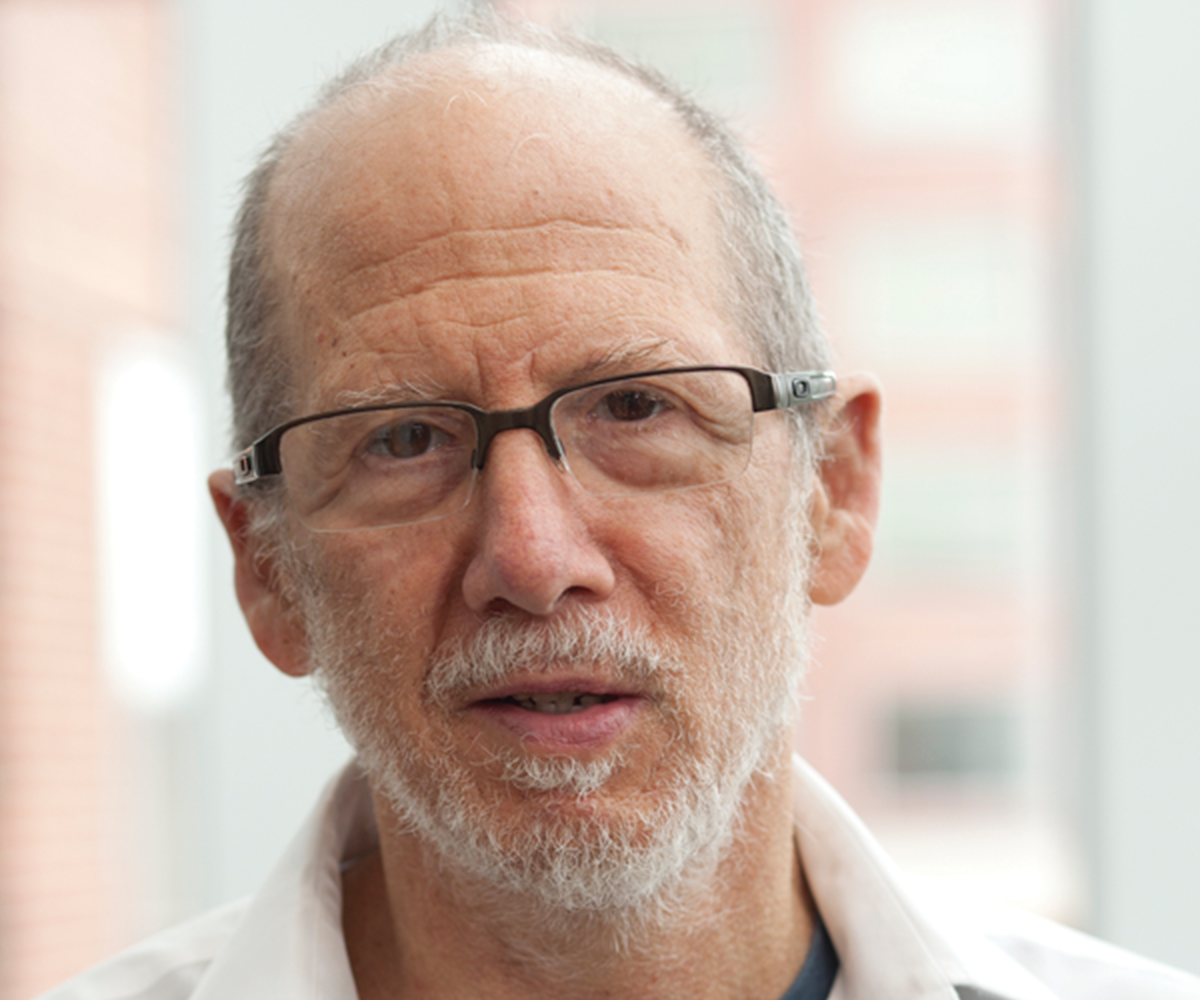
Each of the two primary modes of T cell engineering used for cancer therapy—chimeric antigen receptors (CARs) and engineered T cell receptors (TCRs)—has its limitations. CARs, which use the antigen-binding domains of antibodies, have a high affinity for their target antigens but require a lot of antigens to be present on their target cells to function effectively. TCRs, meanwhile, detect low levels of antigens, but also have low affinity for their targets. Researchers led by Ludwig Johns Hopkins’ Shibin Zhou and Co-director Bert Vogelstein reported in a July issue of Science Translational Medicine their development of cells equipped with an engineered receptor they call costimulatory synthetic TCR and antigen receptor (or Co-STAR) that combines key elements of both CARs and TCRs. The antigen-recognizing elements of TCRs are replaced in Co-STARs by high-affinity antibody fragments, and costimulatory activating signals within the cell are provided by two modules that drive NF-κB signaling (MyD88 and CD40). Shibin, Bert and their colleagues designed a Co-STAR to target a common p53 neoantigen and showed it kills cancer cells in culture that present very low levels of the neoantigen. They also demonstrated that Co-STAR-bearing T cells expand better and induce more durable tumor regressions in mouse models than T cells equipped with similarly targeted TCRs and the same costimulatory molecules.
Preclinical studies show that Co-STARs combine the advantages of chimeric antigen and T cell receptors for the treatment of tumors with low antigen densities
Science Translational Medicine, 2024 July 10